My friend and I recently had a conversation about when we were students, nurses used to praise us a lot for knowing things. This could be because we did most of our schooling in a different country and view university very seriously, but that’s a conversation for another time. Back then we were like: “hummm you’re praising me for knowing the difference between heart failure and a heart attack? Thanks Sue”. Now we know exactly what they meant. Since I qualified, I came across 2nd and 3rd year students who didn’t what what a normal heart rhythm looks like and that is concerning. Everything I expect my students to know is a combination of knowledge I had when I was a student myself and what I believe would be very valuable for them, but for that, you have to lock in! So, in this post, I will tell you some of the knowledge and skills that you really really should have as a student nurse but will discuss them in more detail later on.
First things first. Different students have different knowledge and skills. This depends on multiple factors such as chosen field of nursing, speciality, experience, organisation etc. For example, a 1st year student who has worked as a support worker for a very long time and is used to doing observations and glucose checks will not have the same knowledge and skills as a 1st year student who has never had patient contact before. Another example: a 2nd year student who had placements in the community, gynaecological ward and theatres will not have the same knowledge and skills as a 2nd year student who had a placement on the stroke ward, colorectal surgery ward and A&E. I remember very well that while I was struggling to insert NG tubes because none of my patients needed it, my other colleagues had done them numerous times. It wasn’t my fault, really. I knew the theory and told my assessors about it. I felt embarrassed that I was going to qualify without having done it at least once but guess what? I got additional training and finally had the chance to do it as a newly qualified nurse, safely and with support of other nurses.
However, there is a set of knowledge and skills I believe every student needs to have regardless of experience, so let’s get into it.
1. Clinical observations
The NEWS 2 chart will be your best friend, but before you grab it, you need to be able to recognise when something is wrong. This being said, I will need you to use assemble all your brain cells to memorise the normal parameters of clinical observations, what abnormal result could suggest and try to preempt nursing interventions (we’ll dive deeper into this later).
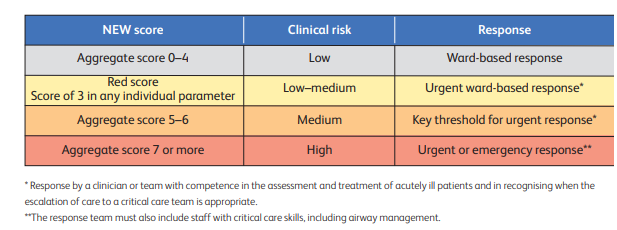
For reference, here’s a table that depicts the NEWS 2 scoring system (Royal College of Physicians, 2017):
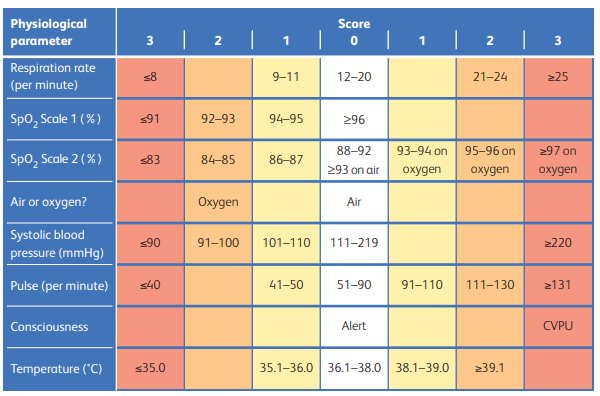
NEWS 2 thresholds and triggers (Royal College of Physicians, 2017):
2. A-E assessment
A-E assessment is a skill that every nurse should have.
Failing to identify and respond promptly to a patient’s clinical deterioration poses a major risk to patient safety and can result in serious consequences, including avoidable mortality (NHS England, 2025). Early recognition relies on conducting a comprehensive patient assessment. The ABCDE method—Airway, Breathing, Circulation, Disability, and Exposure—is the recommended framework for assessing deteriorating patients (NICE, 2007 & UK Resuscitation Council, 2021) and forms a core component of the Recognising and Managing Deterioration programme. This systematic approach also underlies the NEWS2 scoring system, which is intended to complement clinical judgement. By following ABCDE in sequence, healthcare providers assess and address life-threatening issues at each stage before progressing to the next.
3. Diabetes: Management of hypo- and hyperglycemia
Diabetes UK (2025) estimates that in 2023-24, more than 5.8 million people in the UK were living with diabetes, which is an all-time high. When broken down, their data shows that almost 4.6 million people in the UK live with diabetes diagnoses and nearly 1.3 million people could be living with type 2 diabetes who are yet to be diagnosed. Not surprisingly, the RCN (2023) believes that around one in six hospital beds are occupied by a person living with diabetes. This means that there is a very high chance that you will be looking after a lot of patients with diabetes throughout your placements and career. Therefore, knowing about the condition and complications associated to are key to keeping your patients safe.
What is diabetes?

“Diabetes is a long-term condition. People with diabetes experience high levels of glucose in their blood because their body is unable to process glucose properly. This could be because their pancreas doesn’t produce any or enough insulin (insulin deficiency), or because the insulin they’re producing doesn’t work properly (insulin resistance).
There are different types of diabetes:
In type 1, the person is no longer able to produce any insulin and must inject it for the rest of their life. If a person with type 1 diabetes does not have access to their insulin, this can be a life-threatening emergency.
Type 2 diabetes is the most common form, and involves insulin deficiency or resistance. It can be managed through a combination of lifestyle changes and regular monitoring, but some patients need oral glucose therapies and/or insulin injections.
Rarer types of diabetes include gestational diabetes, which develops during pregnancy, and type 3c diabetes, which develops when the pancreas has been damaged.” RCN, 2023.
Hypoglycemia
Hypoglycaemia occurs when blood glucose levels is below 4mmol/L (NHS, 2025a). A hypoglycemia episode can happen quickly and be very dangerous therefore it is important to understand the signs and symptoms and treat it correctly. The most common symptoms are sweating, feeling shaky, being anxious or irritable, feeling disorientated, blurred vision, palpitation and fast heart rate.
Please refer to your local guidelines for specific advice. NHS hospitals normally have a “Hypo Box” which should be readily available, so make sure you know where it is kept in your clinical area. However, in general, as per the National Institute for Health and Care Excellence (NICE, 2025a):
“Any patient with a blood-glucose concentration less than 4 mmol/litre, with or without symptoms, and who is conscious and able to swallow, should be treated with a fast-acting carbohydrate by mouth. Fast-acting carbohydrates include Lift® glucose liquid (previously Glucojuice®), glucose tablets, glucose 40% gels (e.g. Glucogel®, Dextrogel®, or Rapilose®), pure fruit juice, and sugar (sucrose) dissolved in an appropriate volume of water. Oral glucose formulations are preferred as absorption occurs more quickly. If necessary, repeat treatment after 15 minutes, up to a maximum of 3 treatments in total.”
“Hypoglycemia which causes unconsciousness is an emergency. Patients who are unconscious, having seizures, or who are very aggressive, should have any intravenous insulin stopped, and be treated initially with glucagon. If glucagon is unsuitable, or there is no response after 10 minutes, glucose 10% intravenous infusion, or alternatively glucose 20% intravenous infusion should be given.”

Hyperglycemia
When blood glucose levels are too high, this is called hyperglycemia. For many people a level above 7mmol/l before a meal would be a hyper, but target levels can be different for everyone and should be individually agreed by the patient and their healthcare team (Diabetes UK, 2024). If the blood sugar level is slightly high for a short time, emergency treatment is not needed. But if it continues to rise you may need to act fast to avoid developing diabetic ketoacidosis (DKA) or hyperosmolar hyperglycaemic state (HHS). Diabetes management is be complex and there are multiple guidelines and protocols that need to be followed but essentially, what you’re expected to know is that, if you want to bring your patient’s blood sugar down (NHS, 2025b):
– Administer diabetes medicine they’ve been prescribed, as advised by the doctor or diabetes team
– Encourage and educate your patients on the importance of avoiding eating too much sugary or starchy food
– Encourage and assist your patient to try finding ways to manage stress
Additionally, escalate to a senior nurse/ medical team if your diabetic patient experiences the following as they might be signs of DKA or HHS (NICE, 2025b):
– Nausea and vomiting
– Abdominal pain
– Shortness of breath
– Excessive thirst (polydipsia)
– Excessive urination (polyuria)
– Lethargy, drowsiness, and/or confusion
You are not a diabetes specialist nurse nor I expect you to have the knowledge of one, but in summary, know that if your patient’s blood sugar is dangerously low, this is BAD but don’t panic- give sugar and hope for the best. If your patient’s blood sugar is dangerously high, this is also BAD but try not to panic- give insulin and hope for the best.
I apologise for the long post but I hope it was helpful. See you later alligator 😜
References
Diabetes UK. (2024). Hyperglycaemia (Hyper). https://www.diabetes.org.uk/about-diabetes/looking-after-diabetes/complications/hypers#treat
Diabetes UK. (2025). How many people in the UK have diabetes? https://www.diabetes.org.uk/about-us/about-the-charity/our-strategy/statistics#:~:text=We%20estimate%20that%20more%20than,living%20with%20overweight%20or%20obesity.
NHS. (2025a). Low blood sugar (hypoglycaemia). https://www.nhs.uk/conditions/low-blood-sugar-hypoglycaemia/
NHS. (2025b). High blood sugar (hyperglycaemia). https://www.nhs.uk/conditions/high-blood-sugar-hyperglycaemia/
NHS England. (2025). ABCDE Approach. https://www.e-lfh.org.uk/programmes/abcde-approach/
NICE. (2007). Acutely ill adults in hospital: recognising and responding to deterioration. https://www.nice.org.uk/guidance/cg50
NICE. (2025a). Hypoglycaemia. https://bnf.nice.org.uk/treatment-summaries/hypoglycaemia/
NICE. (2025b). When should I suspect a hyperglycaemic emergency?. https://cks.nice.org.uk/topics/diabetes-type-2/diagnosis/when-to-suspect-hyperglycaemic-emergencies-dka-hhs/
RCN. (2023). Diabetes: the essentials for non-specialists. https://www.rcn.org.uk/magazines/Clinical/2023/June/Diabetes-essentials-for-non-specialist-nurses#:~:text=Diabetes%20affects%20around%204.7%20million,a%20person%20living%20with%20diabetes.
Resuscitation Council UK. (2021). The ABCDE Approach. https://www.resus.org.uk/library/abcde-approach